Seeing Double
- Jeanette Luna
- May 21, 2024
- 13 min read
by Sabrina Hsu
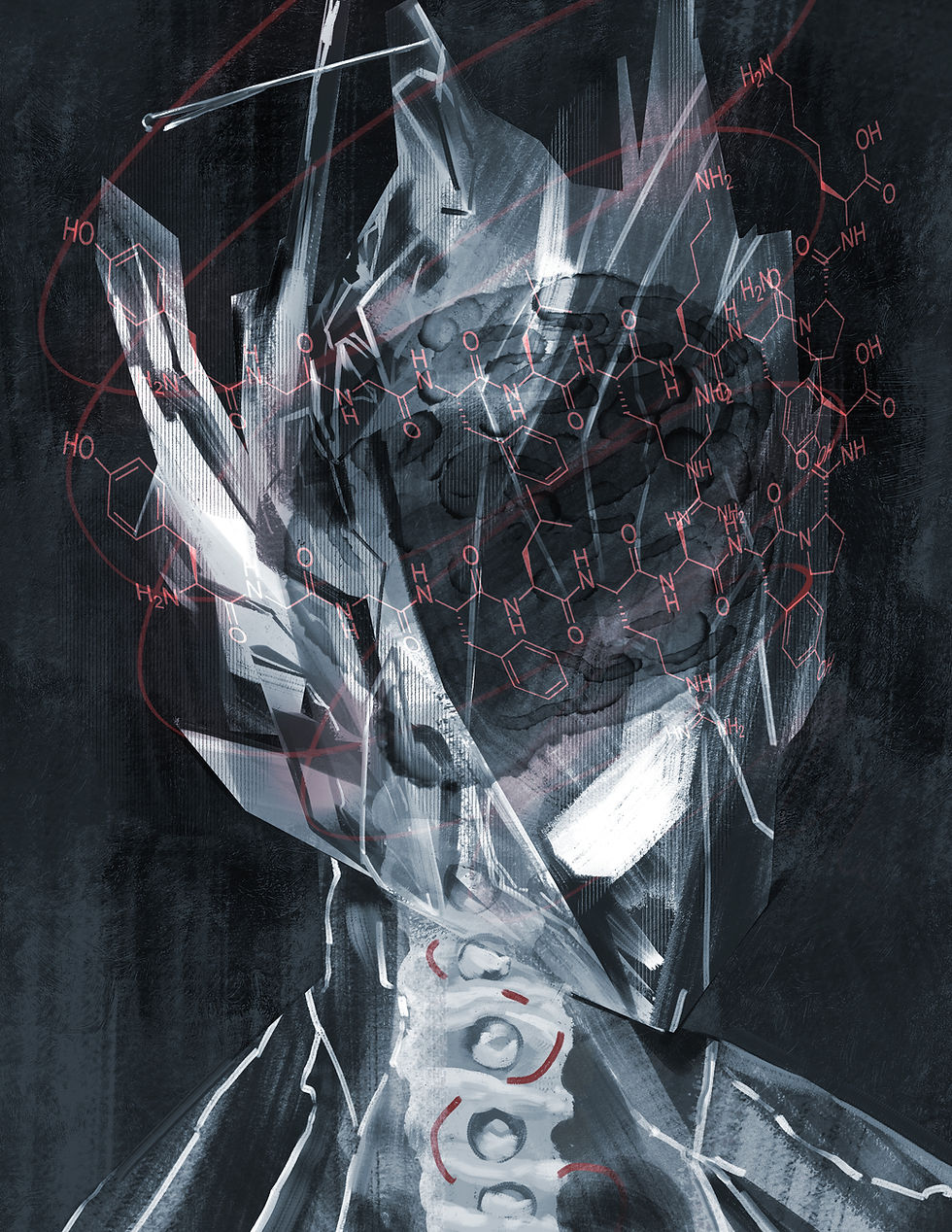
art by Caitlin O’Neil
As a 19th-century Irish housewife, Bridget Cleary raised eyebrows—in life and especially in death. Beautiful, unconventionally independent, and possessing entrepreneurial savvy, she lived apart from her husband, Michael, and ran her own business as a seamstress and hatmaker [1]. When Bridget went missing in March 1895, there was something odd about Michael’s behavior—perhaps his agitated need to confess to a priest or the mournful vigils for a wife he claimed ran away— which led police to suspect foul play. After scouring forests and dragging creeks to no avail, one sergeant stumbled upon incongruously hacked thorn bushes in a field. There, beneath the shrubbery and a thin layer of clay, lay Bridget Cleary. Unclothed aside from her stockings, Bridget’s corpse bore nightmarish marks of violence [1]. How did this happen?
The full story emerged after Michael Cleary and other suspects were put on trial for murder. In early March, Bridget fell ill with bronchitis, an inflammatory lung infection that was the main cause of mortality in England at the time [2]. Her condition worsened so rapidly that her father sent for a doctor and her husband a priest [3]. As Bridget’s condition deteriorated, Michael not only refused her all prescribed medicine but further administered increasingly horrific folk “remedies.” Along with several accomplices, Michael forced Bridget to consume vile, ineffective concoctions, doused her with urine, and then strangled and burned her to death. Why? Per testimony from the group of perpetrators, those acts of torture were an exorcism [3]. They believed that the “real” Bridget had been supplanted by a changeling—an identical impostor left in place after an individual is abducted by faeries [4].
While that may seem an outlandish claim from a modern perspective, changeling myths are deeply rooted in Irish folk culture [5]. Variations of the changeling archetype appear in traditional tales throughout Europe. Irish faeries, Slavic Mamuna spirits, Nordic trolls, Spanish Xanas nymphs, and more have all been depicted to kidnap humans in exchange for one of their own [6, 7]. The abducted individuals are usually young adults or children. This recurrent theme may

have stemmed from the belief that young people are particularly vulnerable to demonic possession, especially when unbaptized [8].
Today, Bridget Cleary is retrospectively (and rather inaccurately) known as the last witch burned in Ireland. Her husband’s motives remain a subject of debate. Was Michael threatened by his wife’s autonomy, self-reliance, and probable reluctance to obey his every whim? Was he a painfully superstitious zealot? Although history has left this unanswered, neuroscience has provided a plausible working theory. In 2006, a paper published in the Irish Journal of Medical Science was the first to suggest a psychiatric origin for Michael Cleary’s actions: Capgras syndrome [4].
Capgras syndrome is a rare but intriguing psychological condition where a person becomes wholly convinced that a close family member, friend, or even pet has been displaced by a physically indistinguishable substitute [9]. Although doppelgänger takeovers have long ensnared the imagination, a recurring motif notably reimagined in Jordan Peele’s Us, the precise mechanics underlying Capgras syndrome remain obscure. This elusive disorder is named after Joseph Capgras, the first psychiatrist to chronicle its symptoms, who aptly termed it “l’illusion des sosies” (illusion of doppelgängers) [10]. In his pioneering article, Capgras records the remarkable case of Madame M., who insisted that her

husband had been murdered and replaced by over 80 disparate impostors over ten years [10]. While Madame M. represents an astonishing figure as the inaugural Capgras patient in academic literature, the delusion is not always as intense and may even be temporary [11].
A wide range of medical conditions have been linked to Capgras syndrome, which further complicates attempts to pinpoint a common causal factor. For instance, Capgras delusions are sometimes observed in dementia patients [12]. However, researchers have found that the prevalence of Capgras symptoms differs among various dementia classifications: two types of dementia (Alzheimer’s and Lewy body) exhibit the hallmark misidentification problems of Capgras Syndrome, while another type (frontotemporal) does not [13]. Although this distinction makes isolating the brain structure that causes Capgras syndrome even harder, it still offers some neurological insight. Alzheimer’s and Lewy body dementia are both closely associated with severe hippocampal degeneration [14, 15]. The hippocampus, an area of the brain heavily involved in memory consolidation and emotional processing, is indispensable in infusing memories with emotional color [16]. As hippocampal deterioration takes center stage for Alzheimer’s and Lewy body dementia patients, memory loss becomes more severe [17, 18]. This can increase the risk that an individual will experience an inability to associate emotions with familiar faces [17, 18]. Given that this inability is a core attribute of Capgras syndrome, scientists have hypothesized that Capgras delusions occur when the hippocampus breaks down, causing the connection between memory and emotion to weaken [9].
To put it simply, scientists suggest that for your brain to identify your naughty little brother correctly, it needs to (a) recognize him and (b) experience a subconscious emotional response, whether it be doting fondness or nagging annoyance [19]. When the connection between those two steps is severed by Capgras syndrome, your brain fails to confirm the identity of your brother due to a lack of emotional familiarity, possibly causing you to experience a kind of emotional blankness and bewilderment [20]. Therefore, you may believe he is an impostor even though your brain recognizes that he looks and acts just like your brother. Imagine gazing at your long-time partner and feeling like they’re a complete stranger, or looking at your mom and feeling certain she’s been replaced by someone who looks eerily similar. This is undoubtedly a disorienting and alarming experience and can be potentially harrowing for both the individual with Capgras syndrome and their loved ones.
Imaging studies of selectively damaged brain regions, or lesions, have allowed scientists to identify several brain areas heavily impacted by Capgras syndrome [21]. One of these regions is the fusiform face area (FFA), a blueberry-sized region specializing in facial recognition [22]. When someone’s FFA is damaged, they may have difficulty recognizing familiar faces, a condition known as prosopagnosia or facial blindness [23]. As issues with recognition also mark Capgras syndrome, this raises the question: is Capgras syndrome simply a manifestation of prosopagnosia? Evidence suggests this is not the case; the recognition issues associated with prosopagnosia and Capgras differ [9, 23]. Unlike individuals with prosopagnosia, who are unable to recognize facial features, Capgras patients can recognize facial features—however, when they do, they are under the impression that these features have been perfectly duplicated [9, 23]. Moreover, facial blindness alone should not automatically make one suspect nefarious impostor activity [24]. This suggests that Capgras syndrome cannot solely be traced back to damage to the FFA, bringing us to another brain region associated with Capgras syndrome: the amygdala [22]. An almond-shaped cluster of cells, the amygdala is an area involved in processing emotions such as fear and anxiety [22]. Patients with Klüver‐Bucy syndrome, which is linked to amygdala injury, exhibit behaviors marked by an unnatural state of zen and a near-complete lack of fear [25]. This disposition contrasts completely with the anxious distrust elicited by Capgras syndrome. Altogether, prosopagnosia and Klüver‐Bucy symptoms suggest that neither FFA nor amygdala dysfunction alone can induce Capgras delusions [25].
It appears that a more promising approach for deciphering Capgras delusions lies in analyzing the exchange pathways that bridge the FFA and the amygdala [22]. When we perceive a face, visual stimuli undergo specialized processing in the temporal lobe, the neural structure overseeing emotional, sensory, and linguistic signals [26]. Within the temporal lobe, the FFA manages facial information and interfaces with the amygdala to assess the emotional significance of each face [22]. Capgras syndrome effectively disrupts these connecting pathways, disabling informational exchange between the FFA and the limbic system. These findings support the idea that an interruption in the normal processing of visual and emotional information is a driving force behind Capgras delusions, resulting in a disconnect between visual and emotional familiarity [22]. When the brain can no longer allot emotional value to a visually recognized face, a sort of cognitive dissonance may occur, forcing the individual to view the person in front of them as an imitation, a fraud [27].
In addition to certain forms of dementia, episodes of Capgras delusions have been documented in conjunction with a wide range of conditions, including epilepsy, multiple sclerosis, and AIDS [28]. Among its diverse co-diagnoses, Capgras syndrome seems especially connected to schizophrenia, a mental disorder where psychosis episodes can distort the perception of reality [29]. A review of 255 Capgras cases showed a 32% overlap with schizophrenia diagnoses [24]. The specific neurological common ground joining the two remains unclear, though scientists are pursuing right frontal lobe damage as a possible contender [30]. Greater progress has been made by studying Capgras patients whose

symptoms arose in concert with traceable brain damage, such as those due to traumatic injuries, a stroke, or carbon monoxide poisoning [11].
Due to the lack of a universally accepted cause for the disorder, a cure for Capgras syndrome has yet to exist. For individuals whose Capgras delusions are a symptom of other disorders, prescribed treatment often involves medications that help ad- dress the underlying condition; these may include antipsychotic drugs for those with schizophrenia or neurotransmitter boosters for those with dementia [31]. The former helps reduce occurrences of hallucination or severe agitation, while the latter temporarily strengthens some cognitive functionality, such as memory [32, 33]. Cognitive behavioral therapy, a form of talking intervention designed to help people recognize their own negative or inaccurate thoughts, can also help patients question and challenge their impostor beliefs in a safe and supportive environment [34, 35].
Researchers are focused on better understanding the disorder’s neurobiological underpinnings and identifying effective treatments [36]. One area of current research is the application of transcranial magnetic stimulation (TMS) to stimulate the FFA and other affected regions [36]. TMS is a non-invasive technique that uses magnetic fields to stimulate the brain [37]. Research indicates that TMS might help improve facial recognition in individuals with Capgras syndrome by modulating the activity levels of impacted areas, but its effectiveness is still being investigated [36]. Despite a lack of targeted treatments for Capgras patients, it is crucial to recognize that Capgras syndrome is a debilitating condition that can shatter one’s quality of life. Individuals diagnosed with Capgras syndrome aren’t just being stubborn or difficult—they’re experiencing a physiological disruption in their brain’s ability to recognize and attach emotions to familiar faces. However, with adequate support and palliative care, they can learn to manage their symptoms and live fulfilling lives.
The tragedy of Bridget Cleary underscores the importance of understanding and addressing the neurological conditions that could have induced Michael Cleary’s irrational beliefs. Capgras syndrome offers a scientific explanation for the delusions that may have played a role in Bridget’s horrific fate. While the specific circumstances of Bridget’s case may never be fully known, it’s clear that undiagnosed and untreated neurological conditions can have serious consequences. By studying conditions like Capgras syndrome and promoting

awareness of their symptoms and effects, we can work toward an enhanced comprehension of the brain to prevent similar tragedies in the future.
It is also crucial to recognize that while Michael Cleary may have been experiencing delusional beliefs associated with Capgras syndrome, his accomplices were likely influenced by a phenomenon known as groupthink. Groupthink occurs when individuals feel pressured to conform to the opinions and decisions of a group, even when those decisions may be flawed or irrational [38]. In the case of Bridget Cleary, the groupthink mentality may have contributed to the escalation of violence and the failure of the accomplices to question Michael’s maniacal behavior. Additionally, we may presume that the group’s actions were influenced by the prevailing misogynistic views of the time period. Bridget was unique for her era as a woman possessing beauty and independence in equal measure. Her success as a businesswoman and her defiance of traditional gender roles may have been perceived as threats to the patriarchal hierarchy. The group’s willingness to believe Michael’s claims and participate in the abuse of Bridget may have also been a manifestation of their learned biases and personal insecurities.
Ultimately, this case is a sobering example of how a combination of factors—including neurological conditions, groupthink, and societal bias—can lead to catastrophic outcomes. By analyzing the complex interplay of these factors, we can gain a deeper understanding of the sociocultural forces that shape our perceptions of difference and inform our actions toward those who are perceived as “other.”
Are you a witch or
Are you a fairy?
Or are you the wife of
Michael Cleary?
So goes an Irish nursery rhyme immortalizing Bridget Cleary [39]. In Bridget’s case, her story’s tragic outcome highlights the dangers of misunderstanding neurological conditions and instead attributing them to supernatural causes. The concept of changelings in Irish folklore was often used to explain behavior that was considered unusual or abnormal, and this belief had devastating consequences for individuals like Bridget, who were perceived as different [8]. Regardless of the geographic source, changeling myths have been used to justify ableist abuse, abandonment, and murder before a scientific understanding of disability was normalized [8]. After all, many of the monsters in stories represent human fears of the unknown [40]. Changelings were sometimes described as exhibiting behavior evocative of neurodivergence [41]. For instance, changelings may display intellectual or behavioral tendencies incongruent with their age and physical characteristics, like fidgeting or unexpected vocalizations [41]. Therefore, some scholars suggest that changeling stories were conceived to reflect prejudice against those with autism, ADHD, dyslexia, Down syndrome, and more [8].
Modern manifestations of changeling fears are rooted more in jest than malice. Today, the narrative archetype lives on as doppelgänger conspiracies, tongue-in-cheek accounts of Avril or Kanye being replaced by lookalikes. These “theories” may be amusing internet fodder, but Bridget’s story demonstrates that the concept of impostor doppelgängers can have serious consequences in the real world. For individuals with conditions like Capgras syndrome, the delusion that an identical stranger has replaced someone familiar is their lived reality. So, while the idea of celebrity clones running amok makes for entertaining blog posts, it should also serve as a reminder of the uncharted complexity of the human brain and how it can shape perceptions of the world that differ from individual to individual. Overall, Bridget Cleary is a cautionary tale about the dangers of misunderstanding neurological conditions. Through continued research and education, we can challenge social prejudice, bolster awareness and understanding, and ultimately improve the lives of those affected by neurological disorders. And hey, maybe we can even debunk some celebrity doppelgänger conspiracies along the way!
REFERENCES:
McGrath, T. (1982). Fairy Faith and Changelings: The Burning of Bridget Cleary in 1895. Studies: An Irish Quarterly Review, 71(282), 178–184.
Widdicombe, J. H. (2020). A Brief History of Bronchitis in England and Wales. Chronic Obstructive Pulmonary Diseases: Journal of the COPD Foundation, 7(4), 303–314. https://doi.org/10.15326/jcopdf.7.4.2020.0135
The “Witch-Burning” at Clonmel. (1895). Folklore, 6(4), 373–384. Re- trieved from https://www.jstor.org/stable/1253745
O’Connell, H., & Doyle, P. G. (2006). The burning of Bridget Cleary: Psychiatric aspects of a tragic tale. Irish Journal of Medical Science, 175(3), 76–78. https://doi.org/10.1007/BF03169179
Yoshida, A. (2006). Fairy Ireland: A Literary History of ” Change- lings”(Yohsei no Ireland:”Torikaego”no Bungakushi).
Lönngren, A.-S. (2015). TROLLS!! FOLKLORE, LITERATURE AND “OTHERING.” Rethinking National Literatures and the Literary Canon in Scandinavia, 205.
Stachowski, K., & Stachowski, O. (2017). Possibly Oriental elements in Slavonic folklore:” mamuna”[part 1]. Studia Linguistica Universitatis Iagellonicae Cracoviensis, 134(2).
Eberly, S. S. (1988). Fairies and the Folklore of Disability: Changelings, Hybrids and the Solitary Fairy. Folklore, 99(1), 58–77.
Coltheart, M., & Davies, M. (2022). What is Capgras delusion? Cognitive Neuropsychiatry, 27(1), 69–82. https://doi.org/10.1080/13546805.2021.2 011185
Capgras, J. (1923). L’illusion des” Sosies” dans un delire systematize chro- nique. Bulltin de Societe clinique de medecine mentale, 11, 6–16.
Garcha, M., Sivakumar, K., Leary, M., & Yacoub, H. A. (2018). Tran-sient Capgras Syndrome Secondary to Bilateral Ischemic Stroke: A Case Report. Cognitive and Behavioral Neurology: Official Journal of the Society for Behavioral and Cognitive Neurology, 31(2), 96–98. https://doi. org/10.1097/WNN.0000000000000152
Sutton, S., Tiruveedhula, V., Jain, U., & Sharma, A. (2014). Capgras Syndrome in an Elderly Patient With Dementia. The Primary Care Companion for CNS Disorders, 16(1), 26742. https://doi.org/10.4088/ PCC.13l01570
Harciarek, M., & Kertesz, A. (2008). The prevalence of misidentifi-cation syndromes in neurodegenerative diseases. Alzheimer Diseaseand Associated Disorders, 22(2), 163–169. https://doi.org/10.1097/ WAD.0b013e3181641341
Ayers, M. R., Svaldi, D., & Apostolova, L. G. (2019). Brain imaging in differential diagnosis of dementia. Practical Neurology.
Frisoni, G. B., Laakso, M. P., Beltramello, A., Geroldi, C., Bianchetti, A., Soininen, H., & Trabucchi, M. (1999). Hippocampal and entorhinal cortex atrophy in frontotemporal dementia and Alzheimer’s disease. Neurology, 52(1), 91–91. https://doi.org/10.1212/WNL.52.1.91
Immordino‐Yang, M. H., & Singh, V. (2011). Hippocampal contribu- tions to the processing of social emotions. Human Brain Mapping, 34(4), 945–955. https://doi.org/10.1002/hbm.21485
Ssonko, M., Hardy, A., Naganathan, V., Kalula, S., & Combrinck, M. (2023). Dementia subtypes, cognitive decline and survival among older adults attending a memory clinic in Cape Town, South Africa: a retrospective study. BMC geriatrics, 23(1), 829. https://doi.org/10.1186/s12877- 023-04536-3
von Siebenthal, A., Descloux, V., Borgognon, C., Massardi, T., & Zum- bach, S. (2021). Evolution of Capgras syndrome in neurodegenerative disease: the multiplication phenomenon. Neurocase, 27(2), 160–164. https:// doi.org/10.1080/13554794.2021.1905850
Roemer, N., Vinogradov, S., & Ochitill, H. N. (2003). Delusions. In M. J. Aminoff & R. B. Daroff (Eds.), Encyclopedia of the Neurological Sciences (pp. 833–837). New York: Academic Press. https://doi.org/10.1016/B0-12- 226870-9/01590-2
Vuilleumier, P., & Pourtois, G. (2007). Distributed and interactive brain mechanisms during emotion face perception: Evidence from functional neuroimaging. The Perception of Emotion and Social Cues in Faces, 45(1), 174–194. https://doi.org/10.1016/j.neuropsychologia.2006.06.003
Bobes, M. A., Góngora, D., Valdes, A., Santos, Y., Acosta, Y., Fernandez Garcia, Y., ... Valdés-Sosa, M. (2016). Testing the connections within face processing circuitry in Capgras delusion with diffusion imaging tractography. NeuroImage: Clinical, 11, 30–40. https://doi.org/10.1016/j. nicl.2016.01.006
Nuara, A., Nicolini, Y., D’Orio, P., Cardinale, F., Rizzolatti, G., Avanzi- ni, P., ... De Marco, D. (2020). Catching the imposter in the brain: The case of Capgras delusion. Cortex; a Journal Devoted to the Study of the Nervous System and Behavior, 131, 295–304. https://doi.org/10.1016/j. cortex.2020.04.025
Haeger, A., Pouzat, C., Luecken, V., N’Diaye, K., Elger, C., Kennerknecht, I., ... Dinkelacker, V. (2021). Face Processing in Developmental Pro- sopagnosia: Altered Neural Representations in the Fusiform Face Area. Frontiers in Behavioral Neuroscience, 15, 744466. https://doi.org/10.3389/ fnbeh.2021.744466
Pandis, C., Agrawal, N., & Poole, N. (2019). Capgras’ Delusion: A Sys- tematic Review of 255 Published Cases. Psychopathology, 52(3), 161–173. https://doi.org/10.1159/000500474
Lilly, R., Cummings, J. L., Benson, D. F., & Frankel, M. (1983). The human Klüver‐Bucy syndrome. Neurology, 33(9), 1141–1141. https://doi. org/10.1212/WNL.33.9.1141
Lu, S. T., Hämäläinen, M. S., Hari, R., Ilmoniemi, R. J., Lounasmaa, O. V., Sams, M., & Vilkman, V. (1991). Seeing faces activates three separate areas outside the occipital visual cortex in man. Neuroscience, 43(2–3), 287–290. https://doi.org/10.1016/0306-4522(91)90293-w
Ellis, H. D., & Lewis, M. B. (2001). Capgras delusion: a window on face recognition. Trends in Cognitive Sciences, 5(4), 149–156. https://doi. org/10.1016/s1364-6613(00)01620-x
Edelstyn, N. M., & Oyebode, F. (1999). A review of the phenomenology and cognitive neuropsychological origins of the Capgras syndrome. Inter- national Journal of Geriatric Psychiatry, 14(1), 48–59.
Halder, A., Panchami, N., & Harshe, G. (2022). A case of schizophrenia with Capgras delusion responded to donepezil. Indian Journal of Psychia- try, 64(2), 219–220. https://doi.org/10.4103/indianjpsychiatry.indianjpsy- chiatry_972_21
Coltheart, M., Langdon, R., & McKay, R. (2007). Schizophrenia and monothematic delusions. Schizophrenia Bulletin, 33(3), 642–647. https:// doi.org/10.1093/schbul/sbm017
Shah, K., Jain, S. B., & Wadhwa, R. (2024). Capgras Syndrome. In Stat- Pearls. Treasure Island (FL): StatPearls Publishing. Retrieved from http:// www.ncbi.nlm.nih.gov/books/NBK570557/
Chokhawala, K., & Stevens, L. (2024). Antipsychotic Medications. In Stat- Pearls. Treasure Island (FL): StatPearls Publishing. Retrieved from http:// www.ncbi.nlm.nih.gov/books/NBK519503/
Malík, M., & Tlustoš, P. (2022). Nootropics as Cognitive Enhancers: Types, Dosage and Side Effects of Smart Drugs. Nutrients, 14(16), 3367. https://doi.org/10.3390/nu14163367
Koc, A. E., Hocaoglu, C., Koc, A. E., & Hocaoglu, C. (2020). What is Capgras Syndrome? Diagnosis and Treatment Approach. In Anxiety Disorders - The New Achievements. IntechOpen. https://doi.org/10.5772/ intechopen.91153
Nakao, M., Shirotsuki, K., & Sugaya, N. (2021). Cognitive–behavioral therapy for management of mental health and stress-related disorders: Re- cent advances in techniques and technologies. BioPsychoSocial Medicine, 15, 16. https://doi.org/10.1186/s13030-021-00219-w
Coltheart, M., Cox, R., Sowman, P., Morgan, H., Barnier, A., Langdon, R., ... Polito, V. (2018). Belief, delusion, hypnosis, and the right dorsolateral prefrontal cortex: A transcranial magnetic stimulation study. Cortex, 101, 234–248. https://doi.org/10.1016/j.cortex.2018.01.001
Terao, Y., & Ugawa, Y. (2002). Basic Mechanisms of TMS. Journal of Clinical Neurophysiology, 19(4), 322. 38.
Baron, R. S. (2005). So Right It’s Wrong: Groupthink and the Ubiquitous Nature of Polarized Group Decision Making. In Advances in Experimen- tal Social Psychology (Vol. 37, pp. 219–253). Academic Press. https://doi. org/10.1016/S0065-2601(05)37004-3 39.
McCULLOUGH, D. W. (2000, October 8). The Fairy Defense. The New York Times. Retrieved from https://archive.nytimes.com/www.nytimes. com/books/00/10/08/reviews/001008.08mccollt.html 40.
Monteiro, B., West, B., & Pizarro, D. A. (2023). Chapter 10 - Monsters and the moral psychology of the “other.” In H. Kapoor & J. C. Kaufman (Eds.), Creativity and Morality (pp. 161–173). Academic Press. https://doi. org/10.1016/B978-0-323-85667-6.00001-3 41.
Albury, W. R. (2011). From Changelings to Extraterrestrials: Depictions of Autism in Popular Culture. Hektoen International: A Journal of Medical Humanities, 3.





Comments