Is It You, or Is It Just January?
- Cecelia Ky-Lan Do
- Jun 15, 2025
- 13 min read
by Noa Yaniv
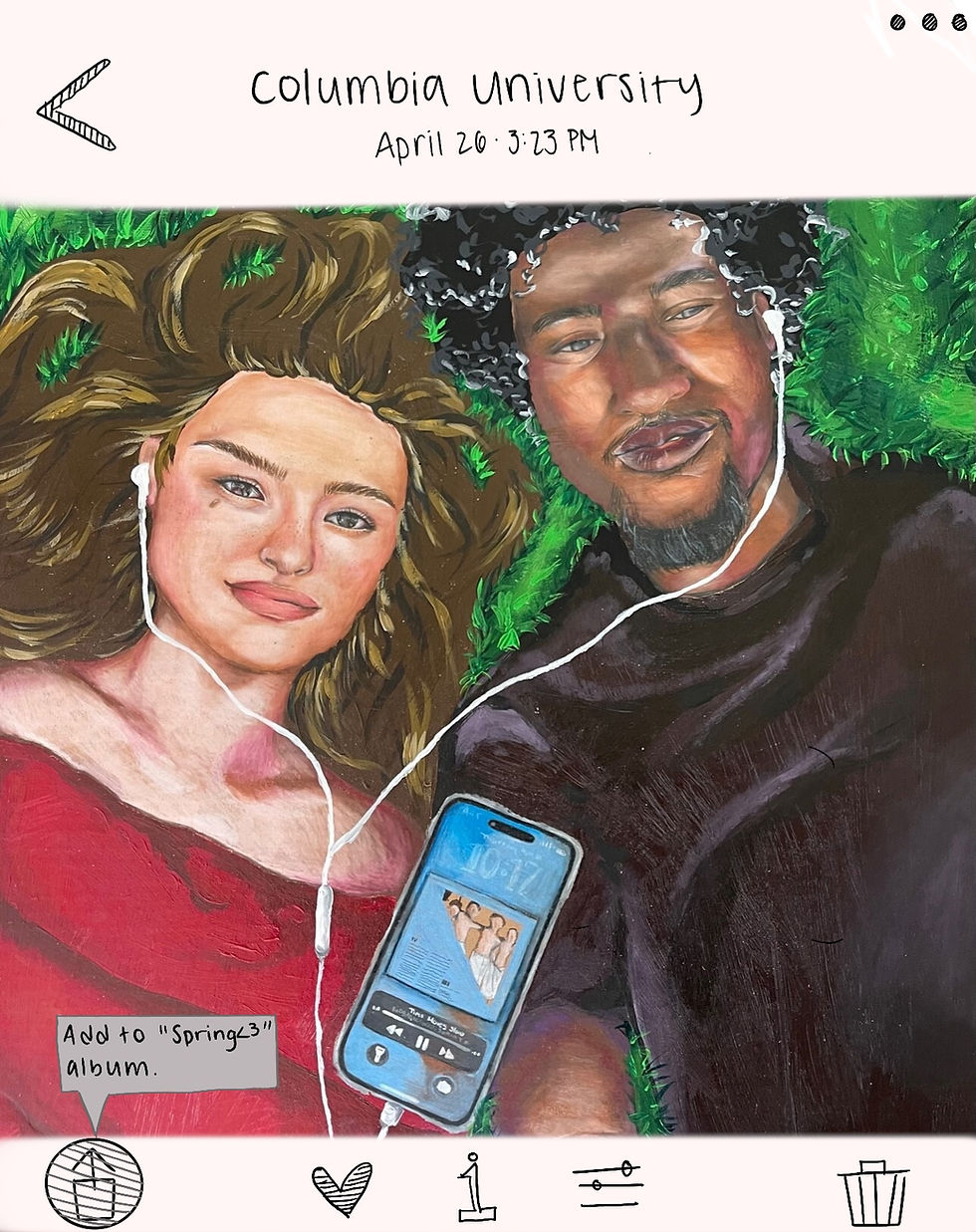
art by Ariel Brown-Ogha

It’s the middle of January, and you start to feel fatigued. You notice your skin looks pale, and suddenly, you find yourself reaching for Trader Joe’s soup dumplings most nights, not out of preference, but from a lack of motivation. You start to wonder: Am I just lazy? Will it stay like this forever? It’s hard to feel stuck in this cycle.
And yet, every year, around mid-March, it’s as if you’ve woken up from a months-long fog of monotony. A walk with a friend feels exciting, and you finally decide to start cooking all of those TikTok recipes you’ve been saving for months. And every year, you swear to yourself that next winter will be different, but it never is. It can make you feel mentally exhausted. But what's actually going on biologically?
Seasonal Affective Disorder (SAD) is a type of depression that occurs during the fall and winter months, triggered by shorter daylight exposure and cold temperatures. The “winter blues” mentioned in countless conversations with your friends are, in fact, a clinical diagnosis [1]. SAD (yes, the acronym is both ironic and true) is classified as a subtype of Major Depressive Disorder (MDD), which involves persistent low mood and other symptoms that interfere with daily life. What sets SAD apart from MDD is its seasonal pattern—symptoms such as sleep disturbances, appetite changes, and feelings of worthlessness typically emerge in colder seasons and usually subside in spring and summer [2, 3]. Interestingly, SAD prevalence increases with latitude. For example, in Florida, only one to two percent of people are affected, whereas this number increases to 10 percent at extreme latitudes like New Hampshire. This geographic trend suggests that the farther you are from the equator, the greater your risk of developing SAD [4].
For college students, especially those struggling with their first East Coast winter (I know I am), these effects can be even more pronounced, making the experience feel more isolating. Populations at higher latitudes report higher rates of seasonal depression, a pattern linked to the disruption of our circadian rhythms—the 24-hour cycle that governs sleep, energy, and hormone release in our bodies [4]. Our brains rely on sunlight to keep these rhythms in sync, but in winter, reduced natural light can disrupt this rhythm, leading to symptoms of depression [5]. Essentially, the body is “stuck” on a different rhythm than the day-night cycle, which makes it difficult to feel energized throughout the day and sleep well at night [6]. At the center of these circadian rhythms is the suprachiasmatic nucleus (SCN), a tiny region in the hypothalamus, often called the body’s “master clock” [6]. Located at the base of the brain, the hypothalamus plays a crucial role in maintaining homeostasis, regulating functions such as sleep, temperature, and hormone release. The SCN receives direct light signals through the retina and uses them to regulate hormone production (like melatonin, which helps control sleep-wake cycles) and synchronize bodily functions with the external environment. When winter daylight shortens, these SCN-driven signals can fall out of sync with the actual day-night cycle, contributing to feelings of fatigue, low mood, and disrupted sleep. So, feeling less motivated and wanting to sleep more isn’t just in your head—it’s an entirely natural, biological response to the season. The phase-shift hypothesis claims that the body’s circadian rhythms are shifted in response to seasonal light changes, which can disrupt mood and energy levels [6]. Essentially, think of your body’s clock as falling out of sync during winter—like jet lag, but stretched out over months instead of just a long flight. On top of that, individual differences in circadian rhythm sensitivity—and even genetic predispositions—can make some people more vulnerable to these season shifts than others.
Now that we understand how seasonal changes affect mood, let’s break down the science behind why winter can feel so emotionally draining. Maybe you’ve heard of serotonin—the brain’s mood-regulating chemical. Serotonin is a neurotransmitter, a chemical messenger in the brain that helps transmit signals between nerve cells, affecting mood, emotions, and other bodily functions [3]. Serotonin plays a key role in maintaining the emotional balance between your body and brain, so when its levels fluctuate, so do your mood and feelings. Serotonin is associated with mood regulation, and its levels are affected by sunlight exposure, which is why we have lower serotonin levels during wintertime [3].
Lack of sunlight isn’t the only culprit; negative air ions (NAIs), which are created when water droplets collide, a fancy way of saying rainfall, are linked to serotonin levels in the brain, influencing mood regulation [7]. Low atmospheric pressure, most common during winter, has been linked to increased impulsivity, migraines, and even suicide [7]. While this change is only one factor among many in depression, evolving evidence and research indicates that abrupt atmospheric pressure drops can correlate with increased stress and headaches, which might exacerbate existing mental health issues. However, further research is necessary to clarify the extent and nature of these effects.
These external factors that influence mood and mental health are often mediated through serotonin, and the serotonin transporter plays a key role in regulating serotonin levels. 5-HTT is a protein that helps clear serotonin from the spaces between cells, known as synapses, by reabsorbing it back into the neuron it was secreted from [8]. The more active 5-HTT is, the more serotonin is removed, leaving less of it available to regulate mood. In healthy individuals, 5-HTT levels follow a natural seasonal rhythm, increasing in the fall and winter and decreasing in the spring and summer. This pattern suggests that serotonin levels naturally decline in colder months, possibly contributing to feeling emotionally low. Think of 5-HTT as a vacuum cleaner on the presynaptic neuron that reabsorbs serotonin from the synaptic cleft; during winter, this vacuum works overtime [8].
For individuals with SAD, this seasonal fluctuation is significantly more extreme. A study using Binding Potential Non-Displaceable (BPND)—a neuroimaging measure that reflects receptor transporter binding, including that of 5-HTT—found that individuals with SAD had a 35.10% increase in serotonin transporter binding in the prefrontal cortex during winter [8].
Higher BPND indicates that serotonin is being cleared too quickly from the synapse, disrupting mood regulation. Think of it like a magnet sticking more strongly to metal: when 5-HTT binds to its receptor more tightly, it removes serotonin more quickly, potentially decreasing mood as a result. Rather than simply having low serotonin levels, those with SAD also experience an increased rate of serotonin removal, which exacerbates their symptoms. This finding challenges the common misconception that SAD is solely attributed to low serotonin levels—instead, your brain removes serotonin too fast in winter due to increased transporter activity. This neurological response leads to your so-called “winter blues” hitting harder and lasting longer [8].
In addition to serotonin imbalance, winter affects other protective mechanisms in the brain; nuclear factor erythroid 2–related factor 2 (NRF2), a protein that helps cells protect themselves from damage, is one such example [4]. NRF2 can be thought of as the brain’s cleanup crew, clearing toxins and repairing cellular damage in response to stressors such as inflammation [4].
However, during the winter, NRF2 activity drops in the brain, leading to more oxidative stress and inflammation, which are two factors strongly linked to depression-like symptoms [4]. At the same time, the immune system ramps up production of inflammatory cytokines–small chemical messenger proteins that help the immune system communicate. Cytokines are like emergency messengers. When properly regulated, they signal the immune system to respond to threats, but when overactive, they can lead to increased inflammation or dysregulated immune responses, triggering chaos. In individuals with major depressive disorder, cytokines such as IL-6 and TNF-α are inflammatory messengers that can exacerbate brain inflammation and intensify depressive symptoms [9].

These cytokines can increase inflammation and serotonin transporter activity, which can also lead serotonin to be cleared from the synapse faster. Furthermore, heightened immune activation can lead the brain to a pro-inflammatory state that compounds depressive symptoms. The combination of increased 5-HTT binding and inflammatory cytokine activity during winter creates a self-reinforcing cycle that contributes to SAD. Additionally, high IL-6 levels have been associated with reduced cortical thickness—the measurement of the brain's outer layer—in key brain regions involved in mood regulation, such as the prefrontal cortex and insula. Think of the cortex like the bark of a tree: when it thins, the brain's ability to regulate mood may weaken. In other words, chronic inflammation isn’t just making you feel worse—it might be physically altering the structure of your brain in ways that contribute to the persistence of SAD symptoms [9].
To better understand how seasonal changes impact brain chemistry, some researchers have turned to the medaka fish, a small freshwater species commonly known as the Japanese rice fish, which scientists often use to study genetic and environmental impacts on behavior [4]. Medaka are particularly valuable as a model organism because they share key biological pathways with humans, including serotonin and dopamine systems [4]. Since these neurotransmitter systems are central to SAD, studying how seasonal changes affect medaka brain chemistry provides insight into the underlying mechanisms of SAD in humans [4]. This fish model helps illustrate how winter-like conditions might similarly affect human brain chemistry, reinforcing the idea that environmental factors, such as reduced daylight, contribute to seasonal mood changes.
In a 2020 study, researchers measured medaka’s sociability and anxiety levels after placing them in two conditions: winter-like 14-hour dark cycles and summer-like 10-hour dark cycles [4]. This study found that medaka fish kept in winter conditions showed less social behavior, more anxiety, and disruptions to their circadian rhythm, mirroring symptoms of SAD in humans. Like many animals, humans experience biological changes in response to winter. So, if you’ve joked with your friends that you feel like an animal in hibernation during the winter months—the truth is, you kind of are. That means feeling less motivated and wanting to sleep more isn’t just in your head; it’s a completely natural, biological response to the season.
Like medaka fish, it’s not uncommon for the shift from high energy to a sudden desire to “hibernate” to feel like it appears out of nowhere. One day, you’re full of energy and feel excited at the thought of leaving your tiny shoebox of an apartment. The next, you feel as though you have no option but to hibernate, wrapped in a blanket, binge-watching Love is Blind and contemplating why the sun sets before 5 PM. This shift in mood is where the Dual Vulnerability Model, proposed by researcher Michael Young, comes in [2]. This model explains why SAD symptoms emerge not all at once, but rather in stages driven by two key vulnerabilities: biological and psychological [2]. First is the biological stage, in which the body physically responds to winter. Then, the psychological stage occurs, in which the mind emotionally responds to these physical shifts [2].
In the biological stage, your body responds to winter’s reduced daylight hours. The sudden craving of carbs and feeling of fatigue (even after 10+ hours of sleep) is a survival
strategy induced by the symptoms of SAD, and are known as vegetative symptoms. These symptoms range from sleep disturbance, to an extreme lack or increase in appetite and loss of energy. Additionally, these vegetative symptoms occur before full-blown depression even hits. Once your body enters its winter slump, the psychological feelings of depression start creeping in. As these biological changes take hold, all of those negative thoughts about yourself that have been building—such as feelings of worthlessness, often accompanied by a TikTok doom scroll, or difficulty concentrating in class—emerge as a reaction to the initial biological changes [2].
This interplay between biology and psychology is further influenced by one’s environment, particularly those who experience a drastic shift in climate. As a California native, I have often been made fun of for my definition of cold by my East Coast friends, and I admit, they are right. College students who have moved from warmer climates to colder climates have been found to exhibit the most significant increase in seasonal depression compared to their peers from New England [10]. This result emphasizes the importance of light, temperature, and location for college students, particularly women [10]. Women are approximately three times more likely than men to be diagnosed with SAD, a disparity that researchers believe may be influenced by hormonal fluctuations and differences in serotonin regulation [11].
Although it’s important to understand the environmental and physiological factors that contribute to SAD, it’s equally important to explore strategies that can help address these seasonal challenges. Two therapies that assist with combatting these seasonal challenges are bright light therapy (BLT) and physical exercise therapy (PET).
You might be wondering, how exactly does staring into a bright light help depression symptoms? Think of your brain like a high-tech internal clock that sometimes lags behind when the seasons change. BLT was developed based on the phase-shift hypothesis, which, as we learned earlier, claims that the body's circadian rhythm shifts in response to seasonal light changes, which can disrupt mood and energy levels [6]. Light exposure, specifically in the morning, helps us simply reset our circadian rhythm, which functions like a clock, targeting the production of melatonin and serotonin [5]. Melatonin is a hormone that regulates our sleep, and darkness triggers its production, which is why we may produce more melatonin than needed during the winter, making us want to sleep more.
Although these two chemicals try to fight within your brain, BLT fights back just as hard but in a quick and efficient manner. BLT is easily done by sitting in front of a lightbox that is about 20 times brighter than regular indoor lighting, an attempt to mimic natural sunlight. Most studies recommend about 10,000 lux (a measure of illumination) for 20-30 minutes in the early morning [12].
So how does this actually work? BLT regulates the SCN, that “biological clock” that controls circadian rhythms. The SCN receives light signals from BLT through the retinohypothalamic tract, a direct pathway that connects the eye's photoreceptors to the brain. This light exposure in the morning helps reset the SCN, aligning the body's sleep-wake cycle with natural daylight [13].
Additionally, BLT tricks your brain into thinking it's a bright summer morning, stimulating serotonin production (your mood booster) and reducing melatonin (the sleep hormone), which helps regulate the sleep-wake cycle and reset your circadian rhythm. This process not only mitigates feelings of fatigue but also elevates your mood and energy levels. [6]. Light exposure has also been found to increase brain-derived neurotrophic factor (BDNF), which is a protein that supports neuroplasticity, learning, and memory formation. Through stabilizing circadian rhythms and neurotransmitter levels, BLT helps keep your prefrontal cortex running smoothly, so your attention span doesn't rival that of a goldfish.
Physical exercise therapy is another proven method for tackling seasonal depression. Though this might feel challenging, physical activity has been found to release endorphins, which are chemicals in the brain that act as natural painkillers and mood enhancers. You might have heard endorphins referred to as the “feel-good” hormones, and this understanding is scientifically correct. But endorphins are just one part of the picture. Exercise also helps us regulate three important neurotransmitters that play a key role in mood regulation: serotonin, dopamine, and norepinephrine. When experiencing depression, these neurotransmitters are often imbalanced, contributing to symptoms like low mood, difficulty concentrating, and fatigue.
Aerobic exercise in particular, which involves activities that increase heart rate and stamina over a long period of time, has been found to be the most effective at boosting endorphins. This can be any sort of simple activity, from a run to a stationary bike at your local gym. Aerobic exercise increases circulation and endurance, supporting your brain. This kind of exercise can also help reduce cognitive symptoms of depression, like poor concentration and mental fog, by improving blood flow to the brain, thus enhancing cognitive function [14]. Exercise also upregulates BDNF, which promotes neurogenesis—the growth of new neurons—in the hippocampus, a brain region that is critical for memory and mood regulation [13]. By enhancing neurotransmitter activity and improving brain circulation, exercise can address both the emotional and cognitive symptoms of depression, improving mood and quality of life simply through increasing the body’s alertness during the day while simultaneously promoting restorative sleep at night.
So the next time you start to be harsh on yourself for your winter mood, remember: your January self isn’t your real self—it’s your seasonal self. Feeling off in winter doesn’t mean you’re failing; it means your brain is responding to seasonal shifts in light, serotonin, and biological rhythms. It’s important to stop blaming yourself for being unmotivated; instead, recognize that this cycle happens every year, and science explains why.
If this sounds familiar, you’re not alone. Seasonal Affective Disorder (SAD) affects millions every year. The National Institute of Mental Health (NIMH) and Mental Health America (MHA) offer great resources to help you understand what’s going on and what actually helps, from therapy to light boxes to lifestyle adjustments. Additionally, the Anxiety & Depression Association of America (ADAA) has tips for managing winter blues that go beyond the basics.
For now, go toss your Trader Joe’s soup dumplings in the microwave, get cozy with a show, and maybe consider investing in a bright light therapy lamp…
REFERENCES:
Seasonal Affective Disorder (SAD). (n.d.). Retrieved April 15, 2025, from https://www.psychiatry.org:443/patients-families/seasonal-affective-disorder
Lukmanji, A., Williams, J. V. A., Bulloch, A. G. M., & Patten, S. B. (2020). Seasonal variation in specific depressive symptoms: A population based study. Journal of Affective Disorders, 261, 153–159. https://doi.org/10.1016/j.jad.2019.10.003
Munir, S., Gunturu, S., & Abbas, M. (2025). Seasonal Affective Disorder. In StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK568745/
Nakayama, T., Okimura, K., Shen, J., Guh, Y.-J., Tamai, T. K., Shimada, A., … Yoshimura, T. (2020). Seasonal changes in NRF2 antioxidant pathway regulates winter depression-like behavior. Proceedings of the National Academy of Sciences of the United States of America, 117(17), 9594–9603. https://doi.org/10.1073/pnas.2000278117
Pinchasov, B. B., Shurgaja, A. M., Grischin, O. V., & Putilov, A. A. (2000). Mood and energy regulation in seasonal and non-seasonal depression before and after midday treatment with physical exercise or bright light. Psychiatry Research, 94(1), 29–42. https://doi.org/10.1016/s0165-1781(00)00138-4
Lewy, A. J., Rough, J. N., Songer, J. B., Mishra, N., Yuhas, K., & Emens, J. S. (2007). The phase shift hypothesis for the circadian component of winter depression. Dialogues in Clinical Neuroscience, 9(3), 291–300. https://doi.org/10.31887/DCNS.2007.9.3/alewy
Brazienė, A., Venclovienė, J., Vaičiulis, V., Lukšienė, D., Tamošiūnas, A., Milvidaitė, I., … Bobak, M. (2022). Relationship between Depressive Symptoms and Weather Conditions. International Journal of Environmental Research and Public Health, 19(9), 5069. https://doi.org/10.3390/ijerph19095069
Tyrer, A. E., Levitan, R. D., Houle, S., Wilson, A. A., Nobrega, J. N., & Meyer, J. H. (2016). Increased Seasonal Variation in Serotonin Transporter Binding in Seasonal Affective Disorder. Neuropsychopharmacology, 41(10), 2447–2454. https://doi.org/10.1038/npp.2016.54
Paganin, W., & Signorini, S. (2024). Inflammatory biomarkers in depression: scoping review. BJPsych Open, 10(5), e165. https://doi.org/10.1192/bjo.2024.787
Low, K. G., & Feissner, J. M. (1998). Seasonal affective disorder in college students: prevalence and latitude. Journal of American college health: J of ACH, 47(3), 135–137. https://doi.org/10.1080/07448489809595634
Rubinow, D. R., & Schmidt, P. J. (2019). Sex differences and the neurobiology of affective disorders. Neuropsychopharmacology, 44(1), 111–128. https://doi.org/10.1038/s41386-018-0148-z
Virk, G., Reeves, G., Rosenthal, N. E., Sher, L., & Postolache, T. T. (2009). Short exposure to light treatment improves depression scores in patients with seasonal affective disorder: A brief report. International journal on disability and human development: IJDHD, 8(3), 283–286. https://doi.org/10.1901/jaba.2009.8-283
Ma, M. A., & Morrison, E. H. (2025). Neuroanatomy, Nucleus Suprachiasmatic. In StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK546664/
Gartlehner, G., Dobrescu, A., Chapman, A., Toromanova, A., Emprechtinger, R., Persad, E., … Wagner, G. (2023). Nonpharmacologic and Pharmacologic Treatments of Adult Patients With Major Depressive Disorder: A Systematic Review and Network Meta-analysis for a Clinical Guideline by the American College of Physicians. Annals of Internal Medicine, 176(2), 196–211. https://doi.org/10.7326/M22-1845






Comments