Going Deep to Treat OCD
- Anjali Nair
- May 1, 2021
- 7 min read
Updated: Feb 25, 2022

We have all seen electricity used in medical TV dramas: the piercing sound of the ECG machine flatlining, nurses fumbling to get the defibrillator machine, shouts of “Charge pass 200!” and “Clear!” as the pads are placed on the patient’s chest and their body is jolted by a strong current. You may have also heard about using electrical stimulation to treat muscle spasms in physical therapy. What if electricity could also be used to treat disorders in the brain? This is exactly what deep brain stimulation (DBS) is all about. If the first thing that comes to your mind when you hear DBS is Neo in The Matrix or Divergent’s simulation room, you are on the right track! The DBS procedure involves surgically implanting electrodes into the brain that are connected to an impulse generator. The electric impulses stimulate the targeted regions and are thought to correct imbalances in neural activity in that region [1]. With its first experimental trial 35 years ago, DBS is a new field of study about which we still have much to learn.
DBS has been successful in treating neurological disorders like Parkinson’s Disease (PD) [2], and, since having received approval for PD treatment from the Food and Drug Administration in 2002, DBS has been experimented for use in a number of other diseases. One such disorder that shows great potential for DBS treatment is Obsessive-Compulsive Disorder (OCD). OCD is an anxiety disorder that is characterized by recurring negative thoughts and uncontrollable behaviors, and it affects 2% of the population worldwide and about two million people in the United States [3]. Contrary to what we might see in the media or in pop culture, OCD symptoms are not limited to the need to keep things tidy. Rather, individuals with OCD are prone to intrusive thoughts and urges, called obsessions, that result in repeated behaviors, called compulsions, in an attempt to alleviate the urges. For example, a person with OCD may develop an obsession with not wanting to adopt a particular characteristic that another person displays, and thus may constantly review their interactions to ensure that they have not exhibited that trait (compulsion) [3]. When these obsessive thoughts begin to hinder their daily functioning, patients may choose to seek treatment.
So, what causes OCD? Research has identified both genetic and environmental factors that lead to imbalances in specific hormones and pathways in the brain [3]. Environmental triggers such as trauma and negative perinatal events (events leading up to and immediately after birth) alter the expression patterns of genes responsible for producing “feel-good” neurotransmitters such as serotonin and dopamine. Although it is not known exactly which genes are being modified, the resultant change in production of these neurotransmitters in certain brain regions has an excitatory impact on those regions [3].
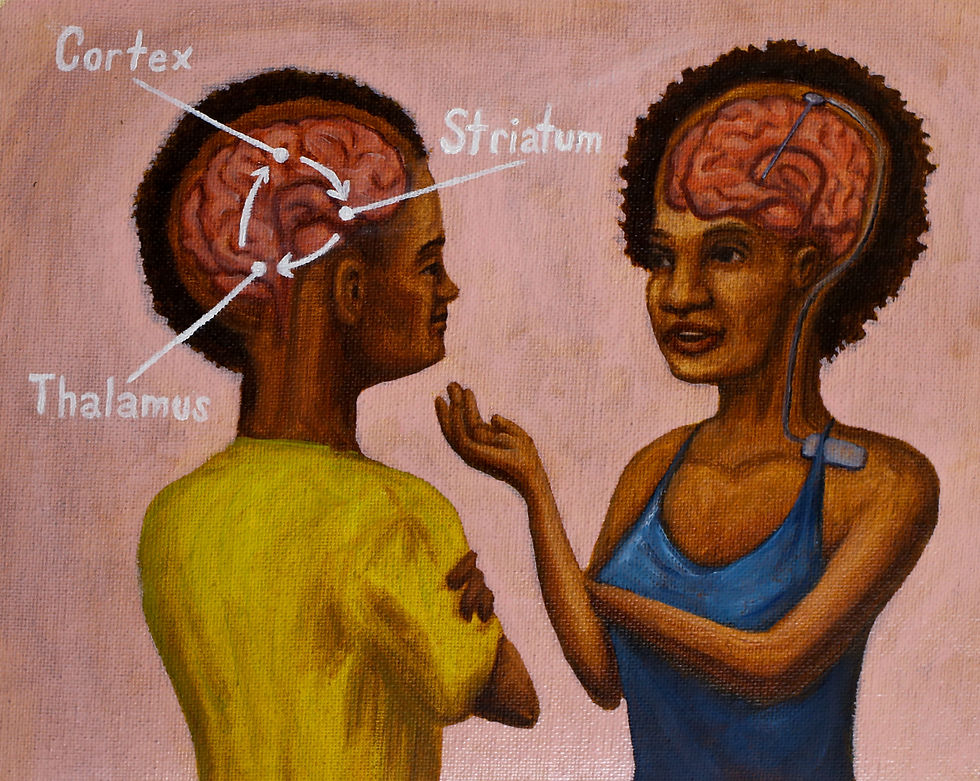
Much of the work on understanding the neural basis of OCD has focused on the cortico–striato–thalamo–cortical (CSTC) circuit, a neural pathway that includes a number of interconnected regions [3]. The CSTC circuit model indicates that there is a pathway of neurons including the cortex (the outermost surface of the brain), the striatum (a subcortical structure), and the thalamus (a second subcortical structure thought to be important for relaying information between cortical regions), which then loops back to the cortex. There are two loops within the CSTC circuit: an excitatory pathway and an inhibitory pathway. In an individual without OCD, the excitatory pathway is modulated, or regulated, by the inhibitory pathway. Think of the excitatory loop as a fan that fuels the flames of the pathway and increases their intensity, while the inhibitory loop is water that works to put out the flames and stops them from spreading. In individuals with OCD, there is an imbalance between the two pathways, causing the excitatory pathway to be stimulated more easily and thus dominate the inhibitory pathway. This modification is correlated with hyperactivation of the orbitofrontal-subcortical pathway, which is responsible for mediating concerns about harm or danger. The excessive excitation is likely to cause obsessions such as concerns about hygiene, danger, and harm in individuals with OCD [3].
These symptoms of OCD can generally be managed by a combination of Cognitive Behavioral Therapy (CBT) and medication. However, these treatments are not effective in roughly 10% of individuals with OCD, who deal with what is known as treatment-resistant or treatment-refractory OCD [1]. For this population, DBS has surfaced in the past few decades as an exciting new potential treatment.

Now, let’s look into how DBS works to treat OCD. Typically, DBS treatment sessions last for several months. Electrodes are placed in a brain region called the anterior limb of the internal capsule (ALIC), located near the center of the brain. Neurons in the ALIC mediate communication between the frontal lobe and the thalamus, two pit-stops in the CSTC pathway [4]. The impulse generator sends electrical signals to stimulate the ALIC and corrects imbalances in the CSTC pathway. The electrical signals are thought to override or inhibit the hyperactivity of the direct pathway, although the exact mechanisms by which this occurs are still unclear [4]. The electrodes’ parameters can be adjusted to be patient-specific, so the pulse frequency, width, and amplitude are tailored depending on how each patient responds to the initial stimulation [1]. This offers customizability and makes the treatment more effective.
Another benefit of DBS is its reversible nature, which allows patients for whom DBS treatment is not working to seek alternative solutions [5]. The reversibility essentially refers to the autonomy of the patient in deciding whether or not to follow through with treatment, as opposed to surgical procedures where the patient is fully committed to the outcome of the surgery [6]. However, this reversibility has been a highly debated topic in the community, because recent evidence has shown that there are non-reversible effects of DBS [6].
For most studies, the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) was used to assess the severity of OCD symptoms, and acted as a quantitative measure of improvement [1]. The Y-BOCS is a checklist that is normally conducted in an interview format, where individuals are asked questions about how much time they spend thinking about their obsessions and how much control they have over them. It then provides ratings for criteria including the presence of obsessions and compulsions, how much time they occupy, and the level of distress they cause.
So far, the results of DBS studies are promising in treating OCD symptoms. In one study conducted on the impact of DBS on OCD, patients showed a median improvement of 37% in Y-BOCS scores [1]. In the follow up study four years after implantation, the improvement is even more significant with a median improvement of 66%. The study reported that stimulation in the ALIC region significantly reduced obsessions, compulsions, and the associated anxiety and depression, and also improved the general functioning of the patients [1].
Despite its promising results, DBS is not without its drawbacks. Some of them are results of the limitations of the research studies themselves, while others have to do with potential limitations of DBS as a treatment option. A number of studies report DBS to have little effect on treating OCD symptoms [7]. It is likely that this discrepancy is due both to differences in stimulation parameters and the sites targeted for the placement of electrodes between studies. Currently, parameters such as the frequency and intensity of electrical stimulation are determined by a trial-and-error method, which can be both time-consuming and inefficient [8]. Most of the studies on DBS for OCD treatment so far have involved fewer than 50 participants. Some studies did not include control subjects, which reduced the reliability of their results. There were also side effects that resulted from the stimulation itself. For example, during stimulation of the ALIC, some patients reported acute mood changes, including sadness, anxiety, and euphoria [4]. However, one study reported that some patients recorded chronic mood improvement, which is a favorable side effect of DBS, as many individuals with treatment-resistant OCD also have chronic depression [4]. Furthermore, there are certain risks associated with the surgical procedure of implanting electrodes, such as hemorrhages and seizures, and dangers associated with the device itself, such as device malfunction, although these are rare. Thus, despite the positive results of most of the studies, the treatment still remains experimental and occurs in controlled clinical trials.
It will be a while before DBS can become a viable treatment option for people with treatment-refractory OCD. Despite DBS having been approved by the Food and Drug Administration for OCD treatment in 2009, the technology still requires significant refining, both in cost and efficiency [9]. For example, a study comparing the costs between rechargeable and battery-replaceable impulse generators found that despite the higher initial cost of the rechargeable generator, it became cost effective in 1.6 years, costing roughly 30,000 USD per year [7]. In order to make DBS treatment for OCD a realistic possibility, more research with larger sample sizes will need to be conducted on the effect of using different stimulation parameters and on stimulating different brain regions. However, the research process is continually evolving. There is a recent trend of moving towards programming the parameters by understanding the physiological properties of DBS [8]. This means that DBS devices will be able to be customized with the specific requirements of the patient in mind, rather than being constrained by cost or electrical engineering. This will increase the efficiency of the procedure by reducing the amount of trial-and-error required [8].
Although the solution might not be as simple as “downloading” new skills into the brain as it is in The Matrix, DBS brings a new exciting development to the treatment of OCD. The promising results of DBS studies so far show that there is potential, but there is still much more to be discovered about DBS. With further research into improving the efficiency and cost of DBS treatment, it will be possible to extend the treatment for more people with OCD who do not benefit substantially from other treatment options.
Luyten, L., Hendrickx, S., … Nuttin, B. (2016). Electrical stimulation in the bed nucleus of the stria terminalis alleviates severe obsessive-compulsive disorder. Molecular Psychiatry, 21(9), 1272-80. Doi: 10.1038/mp.2015.124.
Rodriguez-Oroz, M.C., Obeso, J.A., ...Blercom, N. (2005). Bilateral deep brain stimulation in Parkinson’s disease: a multicentre study with 4 years follow-up. Brain, 128(10), 2240-9. doi: 10.1093/brain/awh571.
Pauls, D.L., Abramovitch, A., … Geller, D.A. (2014). Obsessive-compulsive disorder: an integrative genetic and neurobiological perspective. Nat Rev Neuroscience, 15(6), 410-24. Doi: 10.1038/nrn3746.
Koning, P.P., Figee, M., … Denys, D. (2011). Current Status of Deep Brain Stimulation for Obsessive-Compulsive Disorder: A Clinical Review of Different Targets. Curr Psychiatry Rep, 13(4), 274-82. Doi: 10.1007/s11920-011-0200-8.
Borders, C., Hsu, F., … Bota, R.G. (2018). Deep brain stimulation for obsessive compulsive disorder: A review of results by anatomical target. Mental Illn., 10(20), 7900. Doi: 10.4081/mi.2018.7900.
Pugh, Jonathan (2019). No going back? Reversibility and why it matters for deep brain stimulation. Journal of Medical Ethics, 45(4), 225-230.
Holland, M.T., Trapp, N.T., … Greenlee, D.W. (2020). Deep Brain Stimulation for Obsessive-Compulsive Disorder: A Long Term Naturalistic Follow Up Study in a Single Institution. Frontiers in Psychiatry, 11, 55. Doi: 10.3389/fpsyt.2020.00055.
Lozano, A.M., Lipsman, N., … Krauss, J.K. (2019). Deep brain stimulation: current challenges and future directions. Nat Rev Neurol., 15(3), 148-160. Doi: 10.1038/s41582-018-0128-2.
Food and Drug Administration (2005). Reclaim Deep Brain Stimulation for Obsessive Compulsive Disorder Therapy. Department of Health and Human Services.






Comments